Meet local and national leaders on Weds 7 December, 2022 | 08.45AM - 04.00PM
What is this?
This FREE, face-to-face conference is a chance to recognise and support the work of all nurses in general practice, including advanced nurse practitioners (ANPs)!
Local leaders and national figureheads will be on-hand to join you and your colleagues in:
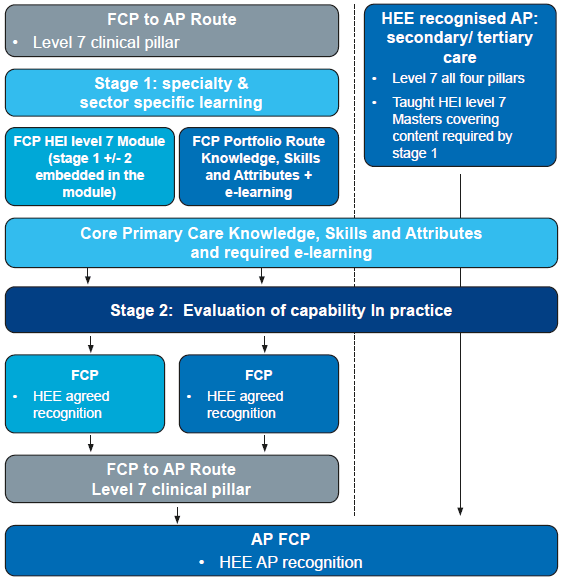
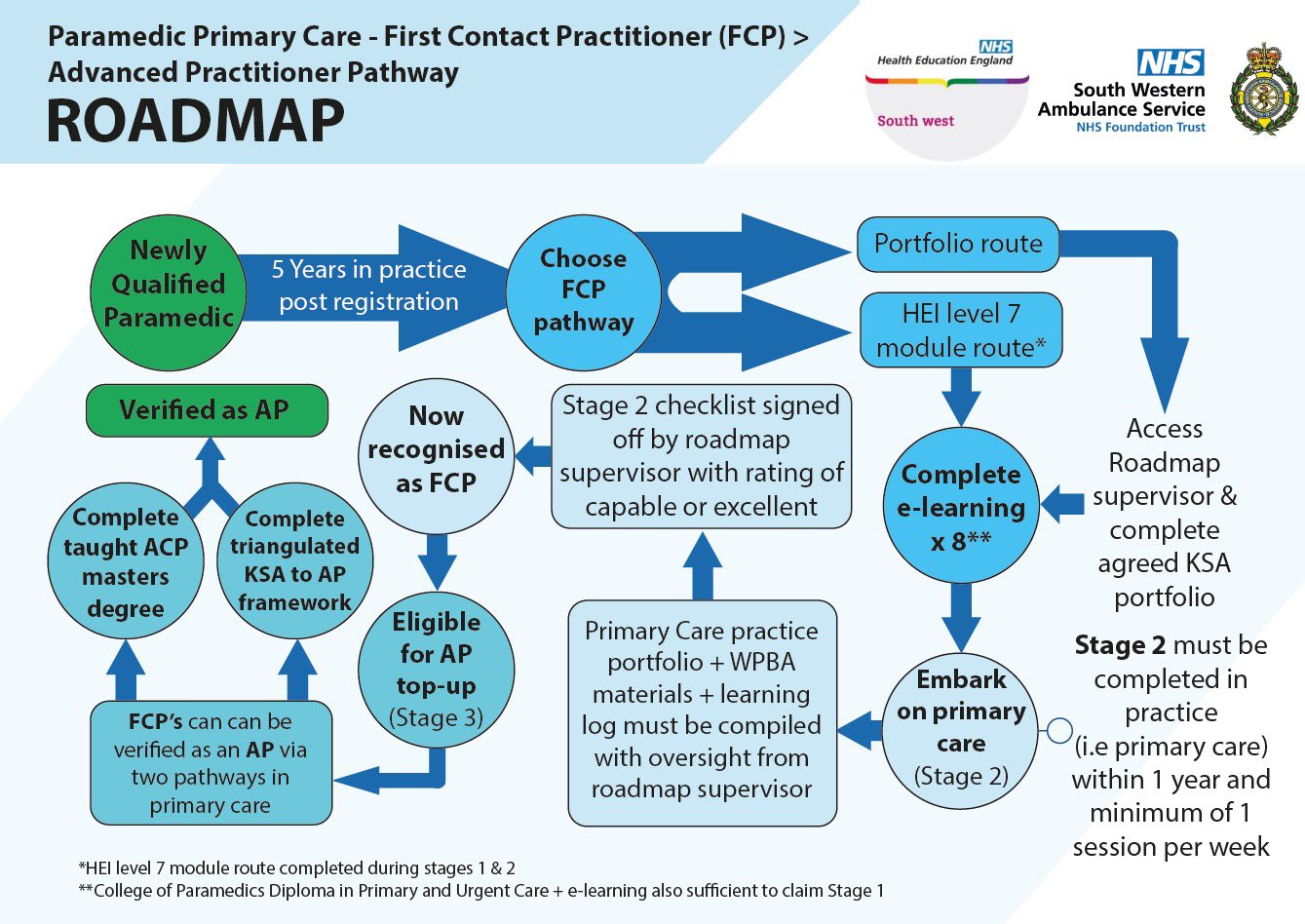
- Exploring Educational Frameworks
- Celebrating Successes
- Sharing Best Practice
- Reflecting on Challenges
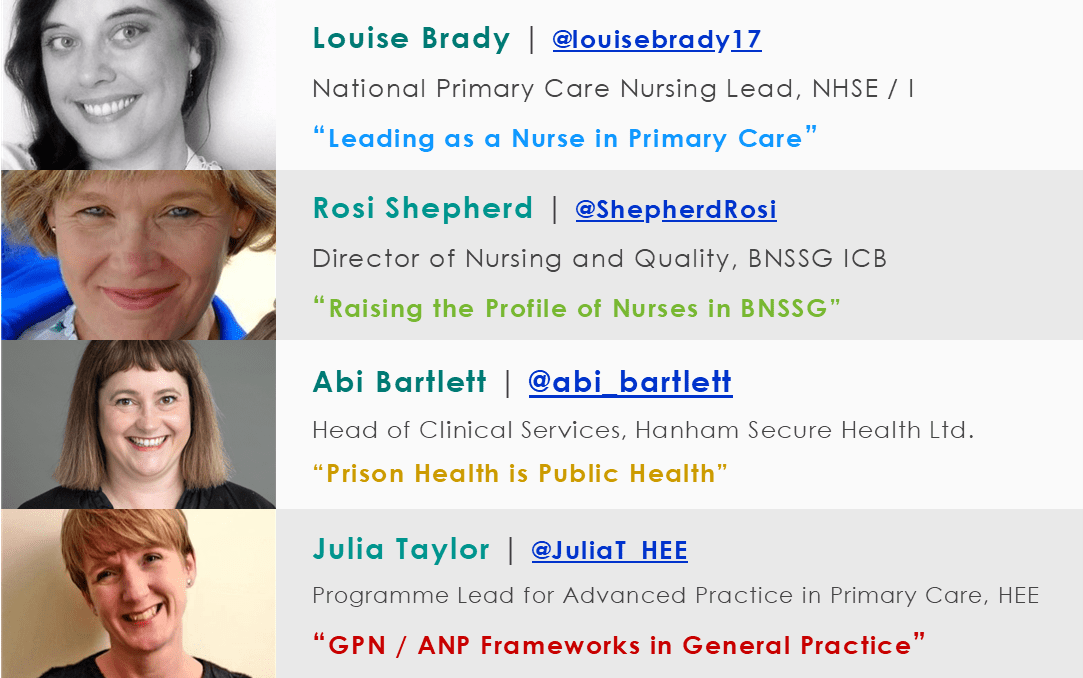
The day’s keynote speakers are:
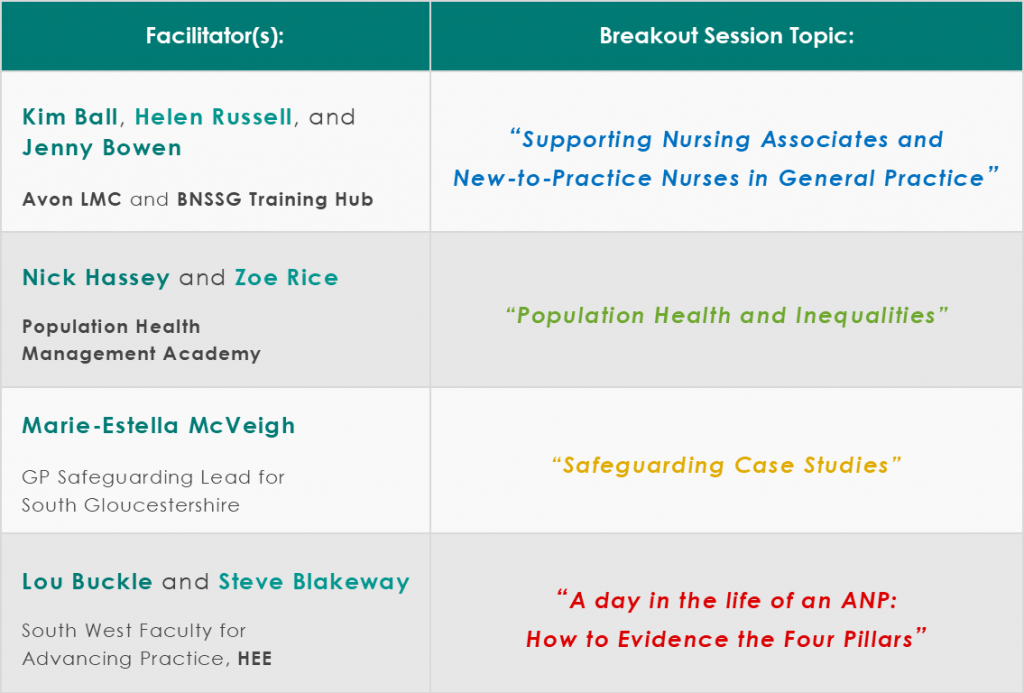
Will there be workshops?
The following breakout sessions will be available. You will need to choose which ones you want to attend — space will be limited, so register interest sooner rather than later!
Where will this be?
Shaftesbury Park,
Frenchay Park Road,
Winterbourne,
Bristol BS16 1LG
Events Calendar
Look for more
|
- - - |
- - - |
- - - |
- - - |
- - - |
- - - |
- - - |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
|
||||||
|
- - - |
- - - |
- - - |
- - - |
- - - |
- - - |
- - - |
|
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
DN_T |
|
|
||||||
You have no events for this day
Look for more
You have no events for this month
Look for more
You have no events for this month
You have no events
stec_replace_summary
stec_replace_location
stec_replace_timespan
Event Info
Location
Schedule
Guests
Attendance
Forecast
Comments
stec_replace_summary
-
stec_replace_titleOrganizer of stec_replace_eventstec_replace_about
-
0
days
-
0
hours
-
0
minutes
-
0
seconds
Event expired
Event is in progress
Location
stec_replace_location
Get Directions
Could not find route!
Details
No schedule
- stec_replace_social
stec_replace_name
stec_replace_about
You are invited to this event!
Places left: 0
-
-
stec_replace_status
stec_replace_name
stec_replace_people
Weather data is currently not available for this location
Weather Report
Today stec_replace_today_date
stec_replace_current_summary_text
stec_replace_current_temp °stec_replace_current_temp_units
Wind stec_replace_current_wind stec_replace_current_wind_units stec_replace_current_wind_direction
Humidity stec_replace_current_humidity %
Feels like stec_replace_current_feels_like °stec_replace_current_temp_units
Forecast
Date
Weather
Temp
stec_replace_date
stec_replace_icon_divstec_replace_min / stec_replace_max °stec_replace_temp_units
Next 24 Hours
Powered by Forecast.io