First Steps into Nursing

A free, 30-minute Q&A session on CPD funding in BNSSG
To help explore the routes to becoming a nurse and the array of opportunities available, Healthier Together will be running a virtual work experience week, this July, for school and college leavers from across Bristol, North Somerset, and South Gloucestershire.
Five live webinars will be hosted each morning from Monday 5 to Friday 9 July (10.00 – 11.00 each time), to cover the following topics:
Career pathways in health and social care | Monday 5 July
“You have to want to be a doctor or a nurse to work in health and care, right? Wrong! There are over 350 jobs in our sector. We show you the huge variety of career pathways — and what you can do straight out of school or college.”
Day in the life of a care worker and nurse | Tuesday 6 July
“What’s a typical day like? Join our webinar to hear a care worker, a nurse, a nursing assistant, and a nurse apprentice talk about their lives at work and the highs and lows of their jobs. There’ll be a chance for you to ask questions, too.”
Patient care and the 6 'Cs' of communication | Wednesday 7 July
“What does it take to care for people for a living? And how do our communication skills make all the difference to the way someone feels? By the end of this session, you’ll find that communication is so much more than the words we say.”
Simulation time! Five health and care situations re-enacted | Thursday 8 July
“What would you do? We share five simulations, including a response to someone having a cardiac arrest in the street and a situation in an emergency department. We talk through the decisions taken at every stage — and their consequences.”
What next? Tips on where to apply and how to shine | Friday 9 July
“Where are jobs advertised? What job titles do I search for? How do I make my application stand out? What preparation should I do for the interview? We explain the recruitment process, plus our tips on how to stand out from the crowd.”
And that’s not all — for more information, please consult the flyer via the button below.
Recent news
CPD Plenary

A free, 30-minute Q&A session on CPD funding in BNSSG
As part of the government’s pledge to secure a sustainable future for the NHS through the Long Term Plan, in September 2019 the Chancellor allocated £1,000 contributions towards the CPD of specific healthcare professionals working in general practice.
In conjunction with Avon LMC, BNSSG Training Hub will be holding a Q&A session for PCN CDs and practice management staff on how to access and use 2021 / 22 funding. Free to attend, and to be held virtually, this session will be on Thursday 17th June, from 13.30 to 14.00. Provided you feel it is appropriate for you, you are welcome to join this session even if you do not identify as a member of practice management staff.
To register your interest in joining, please contact zach.barber@nhs.net.
Recent news
C&SW 2021 Annual Conference

Embracing the Sustainability Challenge
Care & Support West’s annual conference returns for 2021, as a virtual event to be streamed live from Ashton Gate, in partnership with BNSSG Training Hub.
Freely open to all primary, community, and social care staff, this year’s theme is sustainability. Through a series of lightning talks and round tables, speakers will deliver their insights into the well-being, workforce development, and equality and diversity of the care sector — in which the COVID-19 pandemic has revealed huge gaps.
The conference will be split across Tuesday 8 and Wednesday 9 June, with an array of speakers from health and care, and national and local government, on-hand to talk with you — including Sirona Health & Care’s Director of Nursing, Mary Lewis! Make sure to book your spot ASAP.
To view this event’s agenda and register your space, please use the button below.
Recent news
General Practice CPD Funding
Introduction
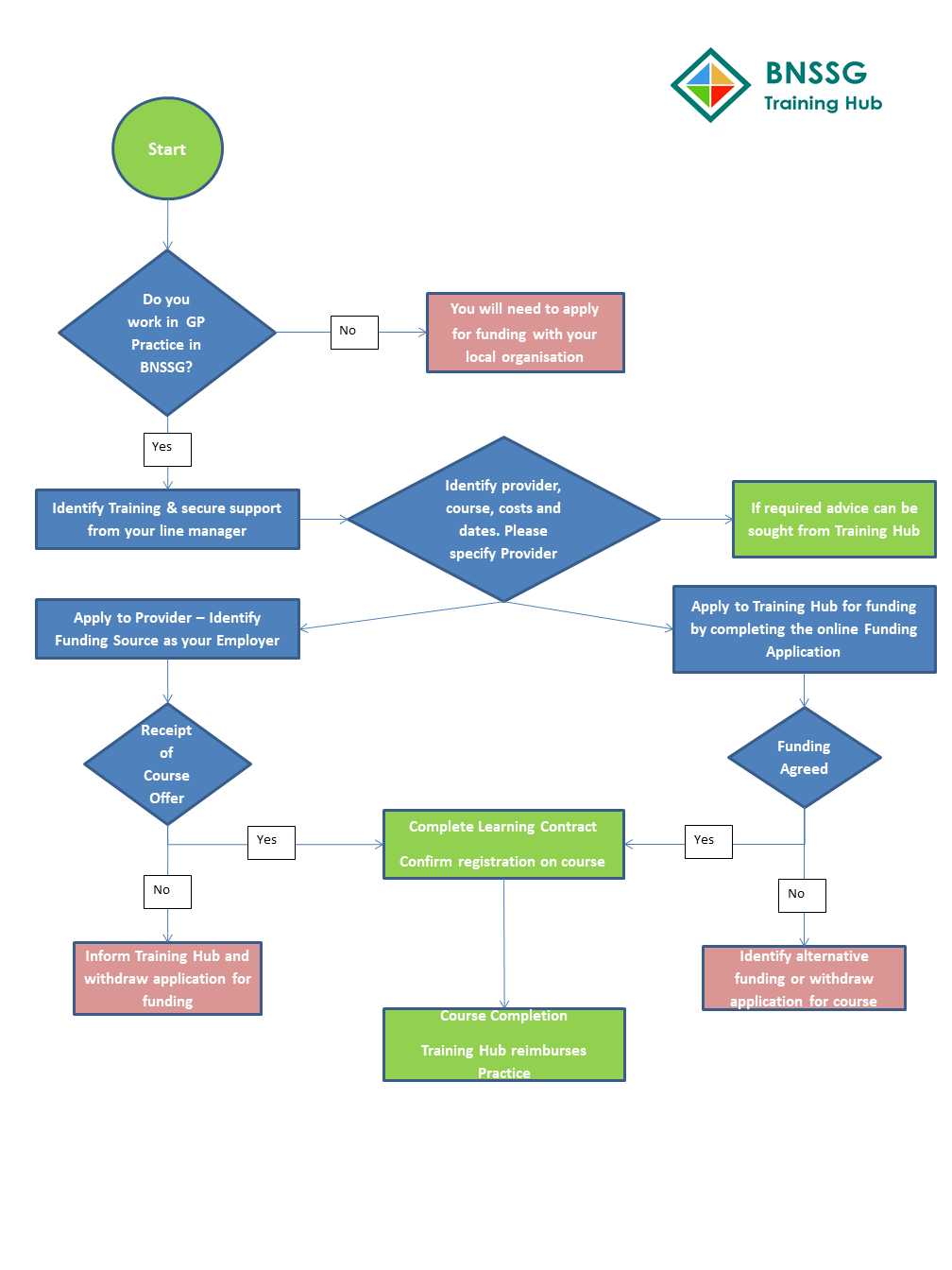
How to Apply
Funding Stream Diagram
Funding Eligibility
Professional Development Advice
FAQs
Introduction
One of BNSSG Training Hub’s core functions is, with a mandate and funding from HEE, to support the recruitment, retention, and development of the local primary care workforce; this can be achieved, in part, by enabling members of the primary care workforce to access and complete the CPD courses and training that they want and need.
We are committed to seeing that all nurses and allied health professionals (AHPs) in BNSSG have access to the £1,000 personal development budget announced back in September 2019, as part of a funding boost for frontline NHS staff. Through this budget, nurses and AHPs may receive up to £1,000 worth of funding over three years, to be put towards their continuing professional development (CPD).
This page will elaborate on how this funding is secured and distributed, and how you can access your allocated amount.
Funding Eligibility
To be eligible for funding from the personal development budget, you must be a member of one of the following roles:
Nurses
- Advanced Nurse Practitioners
- Extended Role Practice Nurses
- Nurse Dispensers
- Nursing Partners
- Nurse Specialists
- Practice Nurses
AHPs
- Nursing Associates
- Paramedics
- Podiatrists
- Physiotherapists
- Therapists
Additionally, you must:
- Be employed by a practice or PCN in Bristol, North Somerset, or South Gloucestershire
- Request funding for an education / training package which is relevant to your role and in-line with the needs of your practice or PCN
- Have the approval of your line manager to complete said education / training package
FAQs
Below are several frequently asked questions (FAQs) about the personal development budget and attendant funding:
Which settings must staff be employed in to be eligible for CPD funding?
Staff in the following settings are eligible for funding*:
- General practice
- Ambulance Trusts
- Foundation Trusts
- NHS Trusts
*The Training Hub only deals with enquiries from staff working in general practice, however.
Staff working in the following settings are excluded from funding:
- Arm’s-length bodies
- CCGs
- Independent sector (inc. orgs that deliver NHS services)
- Social care
- Social enterprises
Is CPD funding available to nursing associates?
CPD funding is available to all registered nursing roles.
What about nurses within federations, as they do not submit onto NHS Digital. How are staff employed on behalf of PCNs and practices considered?
Eligible staff are those working in general practice, and this is in the guidance. The colleagues referred to in the question, although employed on behalf of the PCN, will normally report to NHS Digital via their lead GP practice as part of their workforce return.
Paramedics are AHPs -- won't it be difficult to exclude them?
Paramedics are included and are part of the Health & Care Professions Council’s (HCPC) AHP list.
For more information on the HCPC’s standards for CPD, please click here.
Can CPD funding be used as part payment for a more expensive programme?
If a learning need is evidenced and approved as part of the CPD investment plan, then CPD funding can be used as part payment, yes.
We have recently completed a Training Needs Analysis across our practice / PCN -- will this suffice?
This would require agreement across all practices, the PCN, and the Training Hub. It would be dependent on the training needs analysis being current and relevant.
Does training need to be accredited, non-accredited, or experiential for CPD funding to be considered?
All are eligible.
As we are starting CPD mid-year, can monies be claimed for CPD activity which has already taken place within the financial year?
Yes, but this would need to be evidenced within the application as an identified learning need for a personal development plan.
Will Training Hubs be expected to provide payments to training providers directly, rather than PCNs / practices?
Funding will stream from the Training Hub to PCNs. Applications from eligible members of the workforce will be summarised at PCN level.
Where significant demand is identified for a particular course, the Training Hub may procure at scale based on agreement with the PCN(s). If programmes are procured by the Training Hub, payment will be made directly to the provider.
Is a proportion of this CPD allocation utilised for Training Hub administration costs?
None of the CPD funding will be used to cover Training Hub administration costs. The administration of CPD monies is a core function of Training Hubs, and as such, administration will be absorbed through infrastructure funding.
How does the allocated amount per CCG translate into everyone having access to their CPD amount?
Funding has been allocated down to an individual level using NHS Digital returns. Consideration must be given that CPD funding has been allocated on a ‘point-in-time’ basis. This may not include every member of the current primary care teams, due to workforce movement and incomplete data returns.
Practices are encouraged to complete future data returns to enable more accurate payments in future financial years. If support is required, STP-level Training Hubs can facilitate.
Can monies not spent in-year be carried over?
All CPD monies must be allocated and paid to PCNs / CCGs in-year. The STP-level Training Hub cannot carry CPD funds over into the next financial year.
Will PCNs be responsible for how the CPD funding is spent and administered?
Yes, however PCNs should work with their local Training Hub to develop investment plans.
What happens if staff move during the financial year?
Any funding previously allocated cannot be reclaimed from the individual leader. This CPD funding is excluded from any existing learning & development financial / contractual arrangements. This CPD funding has been allocated regionally by Health Education England (HEE) and no instruction to re-claim monies because of staff movement has been made.
Will personal information be collected and shared?
The Training Hub will be asking for personal staff information to ensure that CPD funds are utilised appropriately, and as agreed. Personal information will be shared with the individual’s PCN for the purpose of confirming funding; it will not be shared with any other party, however.
Aggregate, anonymised information will be shared with Health Education England (HEE) to secure release of funding.
How will personal information be shared while ensuring that GDPR / IG requirements are met?
Personal information will be shared with PCNs by the Training Hub to provide assurances that CPD funds are being distributed fairly. All stakeholders will be responsible for ensuring that GDPR / Information Governance processes are followed, and that personal details are not shared where staff have not consented.
Professional Development Advice
If you would like to talk about your career trajectory and the venues open to you, the Training Hub is here to help you; our ACP Lead, Kerri Magnus, and our Placement Expansion Lead, Kim Ball, are available to meet on a 1:1 basis for 15-30 minutes, to discuss their individual goals and those of their practice / PCN. Line managers are also welcome to book a slot.
To make an appointment, please contact:
Kerri at kerri.magnus2@nhs.net
Kim at kim@almc.co.uk
How to Apply
If you have any further questions, please speak to Kerri Magnus.
GP Short Career Break Project

Have your opinion heard!
Shape support for GPs returning from short career breaks
Dr. Pamela Curtis, GP Fellow for the Hub, invites GPs to participate in a short, anonymous questionnaire to help mould an ongoing project designed to increase support for, and retention amongst, members of the GP workforce.
The survey is aimed at GPs who are (or have been) out of the workplace on a short career break for 3 or more months in the preceding 2 years, or who are planning to take a short career break. It will evaluate perspectives on support available to, and the confidence of, these GPs upon their return to work, with a view to development and implementation of extra support, including ‘return to work’ courses.
This survey is but one part of this work, with a focus group involving a smaller sample of GPs scheduled to be run in May. If you would be interested in participating, please enter your details at the end of the survey or send a message to zach.barber@nhs.net / pamela.curtis1@nhs.net.
The deadline to respond is Thursday 6 May, in advance of the first event we intend to run, informed by this survey and the focus group, in mid-June.
For more information, and to access the survey, please use the buttons below.
Recent news
Study Skills for Nurses & AHPs
Undertaking the portfolio route of HEE’s Roadmap to Practice?
Or in the process of credentialing?
Lacking the skills needed to ace this process at Level 7?
Beginning on Friday 26 May, BNSSG Training Hub is set to run a series of 1-hour study skills workshops, designed to equip delegates with the skills required. Each workshop will provide a constructive environment in which to learn and practice, amidst likeminded colleagues and with a seasoned trainer.
For more information on what each session covers, and the available dates, please expand the boxes below.
Active Reading sessions
Please note: all sessions will run from 12.00 to 13.00 and cover the same material, so you do not need to come to all three.
In this session, you will gain tools to understand how to approach reading literature in a strategic way and making it purposeful. You will also touch on how to approach reading critically, to create ideas and arguments for your assignments and reflections. For this session, you will need to bring with you a journal article, relevant to your work and studies, that you have not yet read.
- Friday 21 May
- Wednesday 26 May
- Tuesday 1 June
Constructing Arguments sessions
Please note: all sessions will run from 12.00 to 13.00 and cover the same material, so you do not need to come to all three.
This session focuses on taking your ideas and reading to construct arguments. Specifically, looking at how to plan your assignments and reflections, and how to structure paragraphs. Please bring with you a title / idea of reflection that you have done some reading / research for.
- Friday 11 June
- Wednesday 16 June
- Monday 21 June
Academic Writing Style sessions
Please note: all sessions will run from 12.00 to 13.00 and cover the same material, so you do not need to come to all three.
This session will focus on how to write academically at Level 7. This includes what is meant by academic style and how to write critically. We will also touch on referencing tools that help to speed up the referencing process and tips on how to edit / proofread your work. Please bring with you a piece of writing that you have completed.
- Friday 2 July
- Wednesday 7 July
- Tuesday 13 July
All sessions will run from 12.00 to 13.00, on the dates listed. Each is standalone, so you can attend as many or few as you like — please note, you will not need to come to all sessions on a given subject, as they will cover the same material.
To register your interest, please contact Kerri Magnus (our ACP Lead) at kerri.magnus2@nhs.net.
Recent news
GPA Certificate course

Free training to step into a versatile, interesting role
HEE is supporting the spread and adoption of the new, emerging GP Assistant (GPA) role, created to relieve some of the pressure on GPs. It has been described as “a cross between a healthcare assistant and a doctor’s personal assistant”. More than 40 GPAs have already been trained across the South West, and with the support of Devon Training Hub, HEE is looking to develop another 40 candidates from general practices across the region – including Bristol, North Somerset, and South Gloucestershire.
Anyone with experience as a practice administrator or healthcare assistant, and with a current Enhanced DBS disclosure, can apply to join the GP Assistant Certificate course. Candidates will need to dedicate one full day a week to the course, which can be achieved flexibly whilst remaining in their place of work; the course will take 6 – 9 months to complete, and is set to commence in April / May 2021. There is no charge for joining the course, and upon completion of the GPA Certificate, participating practices will be eligible for a £1,700 training grant (per candidate) in recognition of the time given to support learners in achieving their competencies.
For more information, please download the flyer and FAQs below. The enrolment form may also be downloaded below.
Recent news
HEE National Paramedic Webinar

An overview of the Paramedic Roadmap
To be held on Tuesday 23 March
Following the HEE Paramedic Roadmap’s publication, HEE will be running a webinar to provide an overview of the roadmap and the supervision requirements on Tuesday 23rd March, from 15.30 to 17.00. This will be an opportunity to hear from a GP’s perspective what the roadmap means for them in primary care and to hear from the College of Paramedics.
The agenda is as follows:
- 15.30: Welcome and open | Andy Collen (Paramedic Subject Matter Expert, HEE / Consultant Paramedic)
- 15.40: Roadmap Overview | Amanda Hensman-Crook (HEE AHP National Clinical Fellow)
- 15.55: Roadmap Supervision and Verification | Julia Taylor (HEE Primary Care Roadmap Supervision and Verification Lead)
- 16.10: College Perspective on the Roadmap | Helen Beaumont-Waters (Primary Care Lead, College of Paramedics)
- 16.25: FCP & AP in Primary Care GP Perspective | Alistair Bavington (GP)
- 16.40: Q&A
- 17.00: Close
For more information, please contact Carrie Biddle (Regional Head of Allied Health Professions, HEE) at carrie.biddle@hee.nhs.uk. To join via Microsoft Teams on the day, please use the button below.
Recent news
Aspiring Leaders in Health & Social Care Nursing

For new-into-post and aspiring nurse leaders in health & social care
Commencing on Wednesday 21 April
Beginning on Wednesday 21 April, a new run of our Aspiring Leaders in Health & Social Care programme will commence. This four-month programme has been put together for any and all new-into-post and aspiring leaders in health & social care in Bristol, North Somerset, and South Gloucestershire — to familiarise them and furnish them with skills, knowledge, and attitudes that will support them in their endeavours.
For 2021, however, we will be offering this programme exclusively to nurses — but as per usual, you may be working in primary, community, or social care. Over its duration, you will join four modules and engage with these pillars of leadership:
- Well-being and resilience on Wednesday 21 April
Facilitated by: Karen Storey (Primary Care Nursing Lead, NHS England), Liz Mallett (CCG General Practice Nurse Lead, BNSSG CCG), Rebecca Howard (from ShinyMind), and Tori McIntyre (Well-being Lead / OD Consultant, SCW CSU) - Harnessing personal strengths on Tuesday 18 May
Facilitated by: sidekick’s Hannah Miller - Navigating the bigger picture on Wednesday 23 June
Facilitated by: Eden & Partners - Application of quality improvement strategies on Wednesday 21 July
Facilitated by: The West of England Academic Health Science Network (WEAHSN)
To apply to join, please use the button below. Applications will be accepted up until 12.30 on Friday 16 April. Should you have any questions in the meantime, please do send them to zach.barber@nhs.net.