What are First Contact Podiatrists?
Podiatrists are highly trained, autonomous practitioners who assess, diagnose, and treat foot and lower limb conditions. As experts in mobility and lower limb health, they use advanced assessment and management techniques to improve overall wellbeing
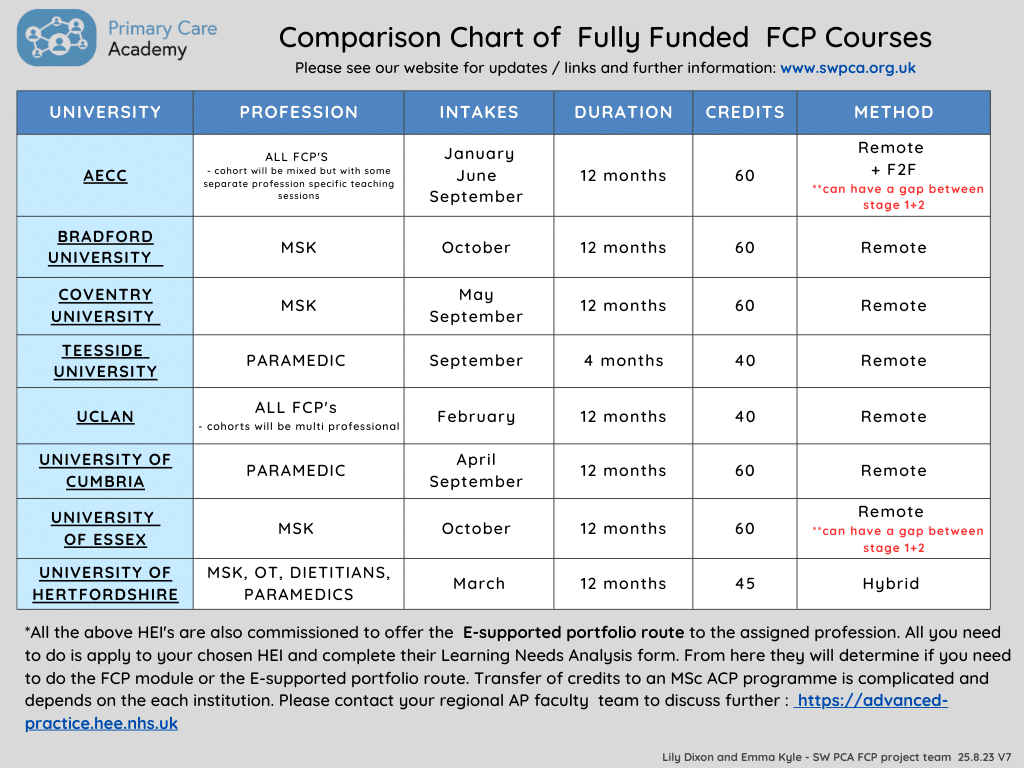
First Contact Practitioner (FCP) podiatrists (also known as First Contact Podiatrists) usually work from GP surgeries and clinics within primary care and can see patients with lower limb conditions without them having seen the GP first. They are usually trained to Band 7 clinical capability in the NHS and demonstrate an extended level of skills, training, and experience.
First point of contact podiatrists:
- Have enhanced level training beyond Band 6 podiatrist in primary care podiatry
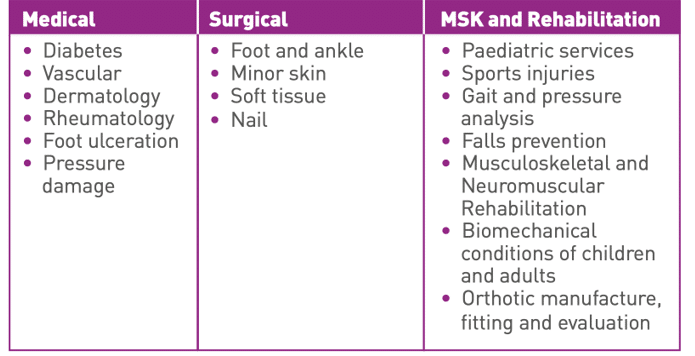
- Uses specialist knowledge of lower limb health across a broad range of clinical presentations spanning musculoskeletal, cardiovascular, neurological, dermatological, or age-related conditions
- Provide personalised self-management advice, formulate initial treatment plans, facilitate shared decision-making, initiate appropriate tests and investigations, and initiate a referral to other services
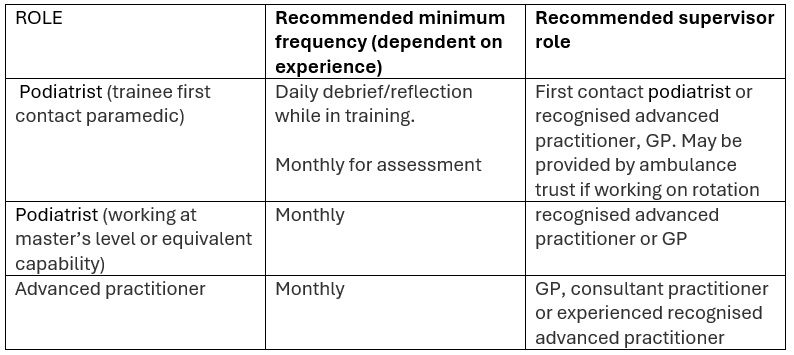
- Can progress from enhanced, to advanced, to consultant-level practice within primary care.
For more information please read NHSE Roadmap to practice and the NHSE Podiatrist in primary care