What are First Contact Dietitians?
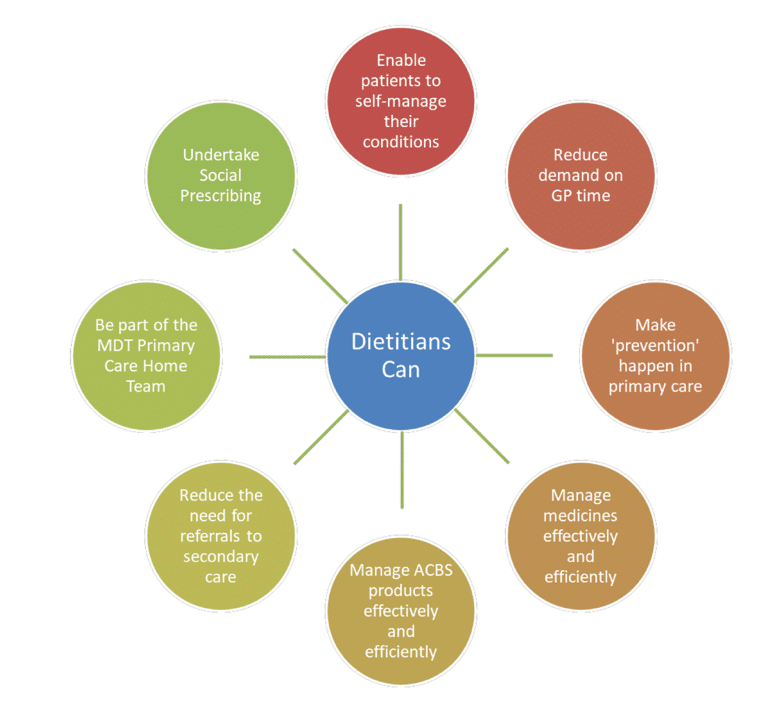
A First Contact Dietitian (FCD) can diagnose medical conditions and then provide suitable dietetic treatment for those conditions. FCDs work in primary care (usually in GP surgeries and health centres). The title ‘First Contact’ points to the fact that patients can make or be given an appointment with an FCD without having to see the GP first.
There are specific conditions that are appropriate for FCDs depending on their knowledge, experience and scope of practice.
Conditions commonly seen include:
- Treating people living with overweight and obesity
- Diabetes
- Frailty
- Gastroenterology, i.e. IBS or coeliac disease
The roles may include other conditions, dependant on a dietitian’s scope of practice. Dietitians working with undifferentiated diagnosis in paediatric populations must have relevant masters level training and education in the management of nutrition and dietetic practice in paediatrics.
For more information please read NHSE Roadmap to practice and the BDA the Association of UK Dietitians :What is a First Contact Practice?