What are First Contact Paramedics?
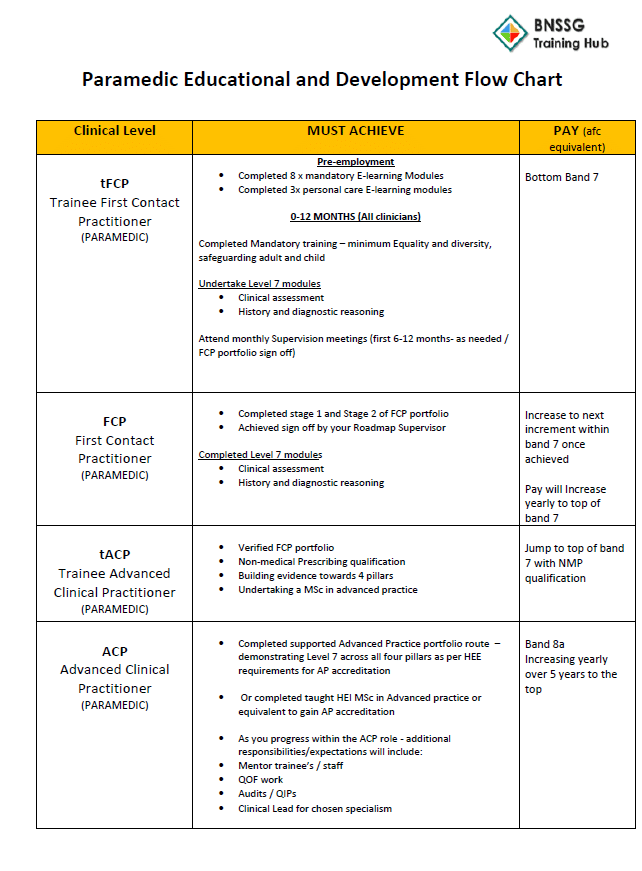
First contact paramedics are autonomous, diagnostic clinicians with experience in handling undifferentiated and unpredictable cases; conducting an array of clinical assessment, diagnostic, and treatment activities; and directing and signposting care. They are at the top of their clinical scope of practice at Agenda for Change Band 7 NHSE Roadmaps to Practice.
As generalists, they can effectively use the medical / biopsychosocial model to assess, examine, treat, and manage patients of all ages, with a variety of undifferentiated and chronic conditions. Their work can involve triaging patients, carrying out telephone and face-to-face consultations, and conducting home visits. They refer patients to GPs for the management of presentations and pharmacology outside their scope of practice.
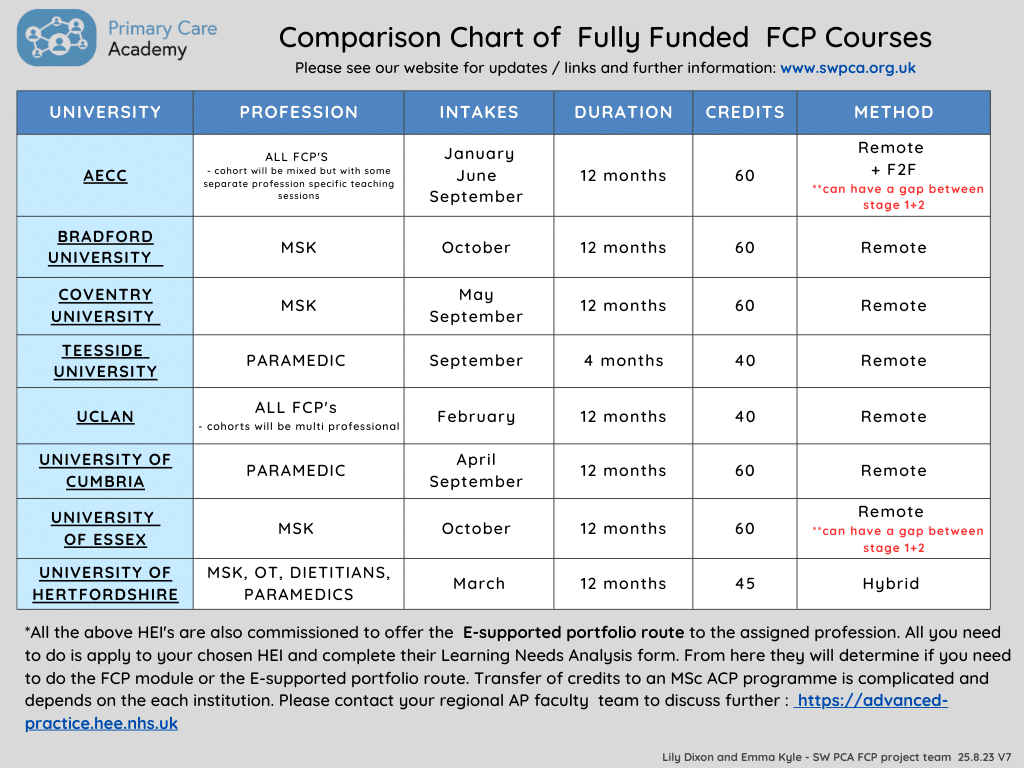
For more information, please read NHSE Roadmaps to Practice and the College of Paramedics’ Employers’ Guide: Paramedics in Primary and Urgent Care.