Social Prescribing Link Workers
What are social prescribing link workers (SPLWs)?
Social prescribing link workers (SPLWs) serve in a non-clinical capacity to help patients and service users take control of their health and wellbeing; they support individuals in creating a shared plan based on ‘what matters’ to them, and to help them connect with local community and voluntary groups and build up their confidence.
Additionally, SPLWs assist local community groups and services in becoming more accessible and sustainable, and support the formation of new ones. They are employed for their listening skills, empathy, and ability to support others.
SPLWs work with a wide range of people, including:
- Those who are lonely or isolated
- Those who need support with their mental health
- Those with complex social needs
- Those with one or more long-term conditions
What benefits can SPLWs bring?
Principally, social prescribing link workers (SPLWs) can help to ease the workload and release time for GPs and general practice nurses (GPNs), by consulting with patients that do not have an immediate need for medical or nursing attention. In fact, 1-in-5 patients come to practice appointments with a non-clinical issue, which SPLWs can also be better-equipped to deal with.
There is evidence that social prescribing can lead to a number of positive health and wellbeing outcomes, including a better quality of life and emotional wellbeing. When implemented properly, SPLWs can support patients and service users in easily connecting with an assortment of local groups and services, including (but not limited to):
- Hospital discharge teams
- Fire services
- Police services
- Job centres
- Social care services
- Housing associations
- Voluntary, community, and social enterprise (VCSE) organisations
What can Personalised Care roles do within primary care?
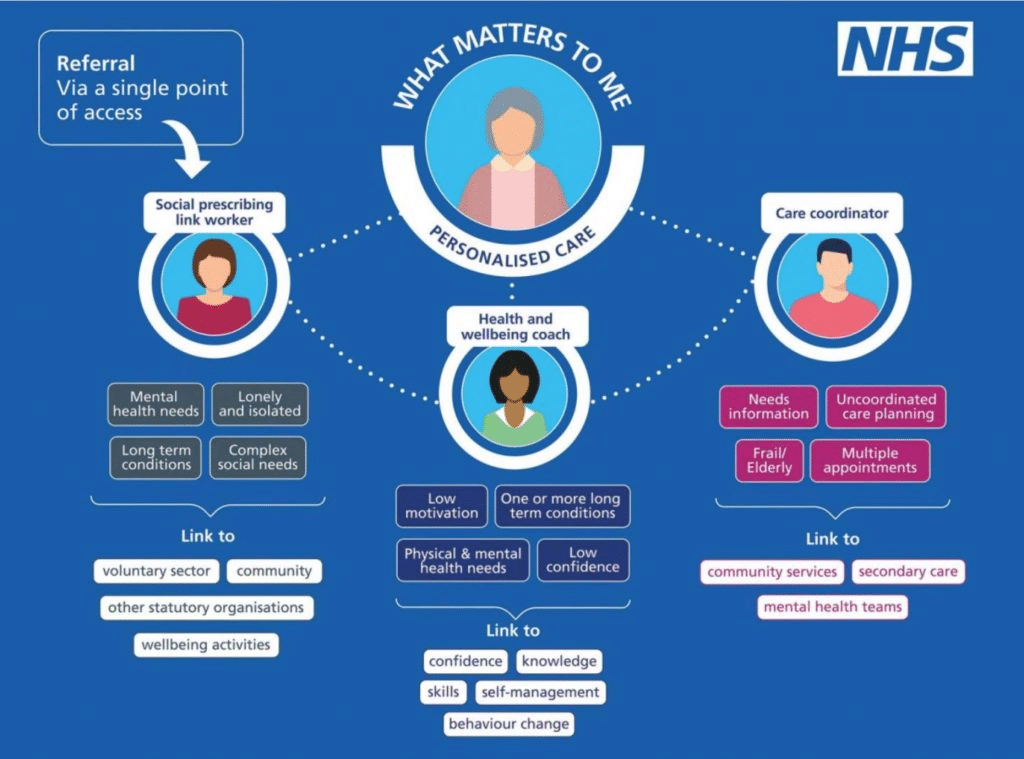
The three additional roles under the umbrella of personalised care aim to support people to improve their health and wellbeing, using a holistic approach and considering what matters to that individual. The infographic below shows a board overview of the 3 roles.
Is funding available for them?
Social prescribing link workers (SPLWs) are one of the Additional Roles Reimbursement Scheme (ARRS) roles. For further information click here.
Are there any case studies?
Social prescribing link worker (SPLW) role case studies can be found here.
What characteristics, training / qualifications, and competencies should they have?
There are no formal qualifications or competencies required to become a social prescribing link worker (SPLW). However, it is recommended that one has the following:
- An understanding of the wider determinants of health, including social, economic, and environmental factors, and their effect on individuals, communities, and families.
- Demonstrable commitment to professional and personal development.
- Experience of partnership / collaborative working, and of building relationships across a variety of organisations.
- Experience of working directly in a community development context, adult health and social care, learning support or public health / health improvement (including unpaid work).
- Knowledge of the personalised care approach.
- NVQ Level 3, advanced level or equivalent qualifications or working towards (recommended by NHS).
- Training in motivational coaching and interviewing, or equivalent experience.
NEW Community Health and Wellbeing Worker Level 3 Apprenticeship – City of Bristol College
This option is ideal for people in roles such as Social Prescribing Link Worker, Care Coordinator, Health Coaches as a Level 3 training option available to them in line with the Network DES recommendations : Additionally, where the Social Prescribing Link Worker does not already have any level 3 qualification (e.g. A level or other equivalent post-16 education), the PCN should ensure that they are enrolled in or, undertaking, appropriate training or an apprenticeship to obtain a level 3 occupational standard, accredited by the Personalised Care Institute for social prescribing link workers with consideration given to the Workforce Development Framework for Social Prescribing Link Workers
72. For those workers who already have a qualification at level 3, a level 3 social prescribing course is recommended but not mandatory.
NHS Careers recommend that SPLWs possess the following characteristics:
- Excellent listening and communication skills
- Empathy
- Emotional resilience
- Open-mindedness
- A willingness to work as part of team
- Good IT and record keeping skills
- A willingness to undertake training and develop skill
- For more information click here
Are there any requirements to receive ARRS funding?
Social prescribing link workers (SPLWs) can be reimbursed via the Additional Roles Reimbursement Scheme (ARRS). However, to be eligible for this funding, there are requirements that SPLWs must adhere to the information outlined in the DES contract.
Any example job descriptions?
An example job description can be found here.
Clinical supervision of SPLWs.
Good supervision arrangements for SPLWs are crucial to ensure they practice safely and effectively. SPLWs should have an initial point of contact within a PCN, a GP supervisor, and monthly clinical supervision with a relevant professional, to manage any emotional issues and to develop their SPLW practice. They may also have a day to day line manager. Supervisors should have relevant experience of the SPLW role, and be supported in their own development as supervisors. For further information click here.
What should practice induction include?
PCNs as employers will want to ensure that all staff are valued and are treated with dignity and respect. Local induction is necessary for onboarding of new SPLWs, and this should promote good working relationships within the PCN, and with other areas of the NHS and external agencies, to help SPLWs feel supported and valued at work. Local induction should also include information for the wider workforce about the SPLW role and appropriate referrals and allow SPLWs to work as part of the MDT effectively.
Employers may wish to include shadowing colleagues, being observed and receiving feedback, and establishing peer support relationships with other SPLWs as part of the onboarding process. It may also be helpful to establish reflective practice at the outset, and employers should think about the learning environment for SPLWs, as with all staff.
Sole SPLWs working in PCNs may need additional support during induction to establish peer support relationships across organisational boundaries. Employers are encouraged to support SPLWs to connect with regional networks and to provide protected time to attend peer support sessions.
The Primary care reference network guide and technical annex includes an induction checklist.
For further information, please head to NHSE.
Further resources
NHS England & NHS Improvement (NHSE / I) have, in their social prescribing link worker (SPLW) induction guide, compiled a list of available support structures and mechanisms — including an online learning community, accessible by contacting england.socialprescribing@nhs.net.
Leadership for Personalised Care.
Social Prescribing Link Worker Induction Pack.
PCN Personalised Care Reference Guide.
Social Prescribing Link Worker PDF.
SPLW Support Matrix including supervision.
BNSSG Training Hub – Training Matrix for Personalised Care staff.
NHSE – Shared decision making.
What is trauma informed practice?
BNSSG ICB personalised care awards.
Green Social Prescribing – The Birch Collective – Jay’s Story