Care Coordinators
What are care coordinators?
Care coordinators work as part of the general practice multidisciplinary team (MDT) to identify people in need of proactive support; this could mean, as a examples, people living with frailty or with multiple long-term physical and mental health conditions. Care coordinators will work with these patients on a 1-2-1 basis, building trusting relationships, listening closely to what matters to them, and helping them to develop a personalised care plan.
As part of this work, care coordinators will review people’s needs and help to connect them with the services and support they require, whether that’s within the practice or elsewhere – for example, community and hospital-based services. They may support people in preparing for or following up clinical conversations they have with healthcare professionals, to enable them to be actively involved in managing their care and supported to make choices that are right for them.
They will work closely with social prescribing link workers and health and wellbeing coaches, referring people to them and also receiving referrals in return.
NHS England Care coordinators.
What can Personalised Care roles do within primary care?
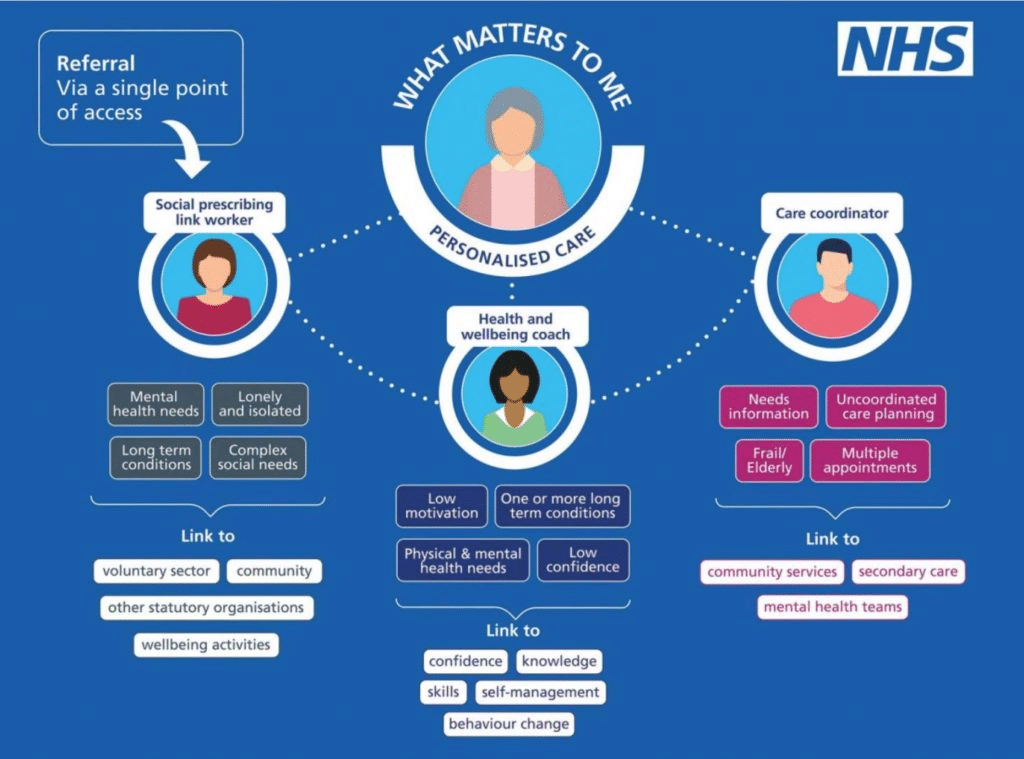
The three additional roles under the umbrella of personalised care aim to support people to improve their health and wellbeing, using a holistic approach and considering what matters to that individual. The infographic below shows a board overview of the 3 roles.
The benefits provided by care coordinators.
The benefits provided by care coordinators, as follows:
- Care coordinators are the patient’s go-to person if their needs change or if something goes wrong with service delivery: the care coordinator ensures that there are no gaps in the patient’s service provision, as many elderly and disabled people with highly complex needs struggle to coordinate with all the relevant services directly on their own
- Care coordinators help improve patient education and understanding, and overall better health outcomes
- They can help patients in avoiding unnecessary appointments, procedures, and tests, and to feel more empowered and actively engaged in their treatment
- A more seamless service provision significantly decreases the risk of the patient deteriorating and thereby reduces the overall cost of care, and the likelihood that additional interventions will be needed in future
- By identifying high-risk patient populations before they incur costlier medical intervention, employers can begin to reduce both practice expenses and total NHS costs
- Employers can gain access to additional data that can reveal practice population health levels and risks; care coordinators glean information about patients’ treatment histories, medication adherence, new symptoms, and management of chronic conditions
What is their scope of practice?
The health and care system is complex and can be confusing and difficult to navigate, especially for those who are vulnerable, frail and/or face health inequalities. The skills and expertise of care co-ordinators support the health and care system in various ways. Please see this link for further information.
Employing a care coordinator.
As with any role in a health and care setting, care co-ordinators should be supported and enabled to thrive in their role. Employers should be clear on the purpose of the role and how it can contribute to meeting people’s needs and neighbourhood/place/system priorities, including objectives around population health management and health inequalities.
Making sense of coordinated care, produced by Health Education England and Birmingham City University, is a useful resource for organisations setting up a co-ordinated care service and includes a useful checklist for developing a co-ordinated care service.
Employers should be confident that they have the necessary resources and support to embed the care co-ordinator in the team. This includes having appropriate supervision arrangements in place, which is essential, and provision for training and ongoing continuing professional development (CPD).
A template recruitment pack has been developed and is a helpful resource for primary care networks (PCNs) and other employers that want to recruit a care co-ordinator (you will need to register for a FutureNHS account to access this template and some of the other resources referenced in this framework). It provides a job description and sets out the skills and responsibilities of the role. Appendix one includes a competency framework for care co-ordinators, which can be used to support recruitment, retention, supervision and ongoing CPD.
Training and requirements.
Care co-ordinators come to the role with a wide variety of transferable skills and experiences. However, a basic level of training is needed before care co-ordinators should take referrals. This is important for all care co-ordinators to work safely and effectively, but particularly for those who have never worked in the NHS before.
Employers should ensure that care co-ordinators have the necessary skills and training before taking referrals. Training falls into two parts:
- personalised care and care co-ordination training
- induction and training specific to the setting the role is working in.
Care co-ordinators should complete Personalised Care Institute accredited training before taking referrals or at the start of their employment, if they have not done this already. Details of the minimum training requirements for care co-ordinators can be found on the Personalised Care Institute website. Two-day accredited care co-ordinator training is a minimum requirement. This course will ensure a developed understanding of the role of a care co-ordinator and where it adds value to people and the system.
In addition, care co-ordinators need to complete Personalised Care Institute accredited online learning courses. They may also find coaching skills and motivational interviewing skills training useful.
Are there any requirements to receive ARRS funding?
Network Contract Directed Enhanced Service – Contract Specification.
Network Contract Directed Enhanced Service Guidance.
Further Network Contract Directed Enhanced Service resources.
Job descriptions, induction and recruitment.
Workforce development framework for care coordinators.
BNSSG Training Hub care coordinator induction and training pack.
Supervision requirements.
Good supervision arrangements for care co-ordinators are crucial. Supervision is key in terms of supporting care co-ordinators to excel in their role and in supporting their ongoing CPD, especially those new to the role who are less experienced.
NHS England carried out a survey of care co-ordinators working in primary care in autumn 2021 to understand their experiences. In the survey, lack of adequate supervision was cited as one of the main reasons for care co-ordinators leaving their role. Employers will have their own resources and arrangements for line management and supervision, including carrying out appraisals.
Organisations that employ care co-ordinators should have appropriate supervision arrangements in place, including a named first point of contact for general advice and support. Supervisors should be experienced members of staff with a good understanding of the role of a care co-ordinator and ideally an understanding of advanced communication skills. It is recommended that supervision should take place on a minimum of a monthly basis (for full time staff) and this could be provided by one or more named individuals. New, less experienced care co-ordinators may need more frequent supervision in the first six months as they learn about the role and the setting they are working in.
Where organisations commission care co-ordinators via a third party arrangement, for example, through a voluntary community and social enterprise sector or other partner, supervision arrangements should be agreed as part of the commissioning arrangement to ensure that appropriate supervision is in place.
Care co-ordinators should be able to discuss patient related concerns (for example, abuse, domestic violence and support with mental health) with a senior member of staff and be supported to follow appropriate safeguarding procedures. Regardless of the setting the care co-ordinator works in, it should be clear who they need to speak to in the first instance about any patient-related concerns.
PCNs employing care co-ordinators should refer to section B5.5 of the Network Contract DES contract specification for specific supervision requirements.
NHS England Supervision requirements
What ongoing support is available for care coordinators?
NHS England & Improvement (NHSE / I) have, in their care coordinator welcome pack, compiled a list of available support structures and mechanisms — including an online learning community, accessible by contacting: england.supportedselfmanagement@nhs.net
NHSE / I Services
Included in their welcome pack for care coordinators, NHS England & Improvement (NHSE / I) have compiled a list of ongoing support and resources, including:
- Online collaboration
- Learning, developmental, and peer support
- Supported self-management mentors
To read it, please click here.
Personalised Care Institute
The Personalised Care Institute has a range of FREE training, resources, and podcasts available for care coordinators.
This includes training covering:
- Core Personalised Care Skills — providing a holistic view of health and care, highlighting the benefits of personalised care, and demonstrating how it improves both health outcomes and patient / clinician satisfaction
- Shared Decision Making
- Personalised Care and Support Planning
The Personalised Care Institute also offers a two-day health coaching course, which allows attendees to discover and develop health coaching mindsets and skills tailored to activation. Feedback suggests that this training is experiential, authentic and immediately impactful.
To find out more, please visit their site here.
Further resources.
Workforce development framework for care coordinators.
Person-Centred Approaches – elearning for healthcare.
FutureNHS Collaboration Platform an NHS England online learning and support community – with Forums, Resources, National Webinar Series & “share and learn” sessions.
NHSE – Shared decision making.
What is trauma informed practice?
BNSSG ICB personalised care awards.

